Brain injuries can be life-altering, affecting individuals physically, cognitively, and emotionally. Understanding the recovery statistics associated with brain injuries is crucial for patients, caregivers, and healthcare professionals alike.
In this post, we delve into the data to uncover insights into brain injury recovery rates, long-term outcomes, and factors influencing recovery.
Brain injury refers to damage to the brain that can result from a variety of causes, including traumatic events such as falls, accidents, sports injuries, or assaults, as well as non-traumatic events such as stroke, tumors, or infections.
Brain injuries are more prevalent than one might think. According to the Centers for Disease Control and Prevention (CDC), an estimated 2.87 million TBIs occur each year in the US, contributing to approximately:
These statistics highlight the alarming frequency with which brain injuries occur and underscore the need for effective prevention, diagnosis, and treatment strategies.
Brain injury can affect physical, cognitive, emotional, and behavioral functions, often requiring ongoing medical care and rehabilitation. Here are some common long-term effects associated with brain injuries:
While many individuals with brain injuries make significant progress during the initial stages of recovery, the long-term outcomes can vary widely.
Some individuals may achieve near-complete recovery, while others may continue to experience residual symptoms or disabilities that impact their daily functioning and quality of life.
In fact, according to the Brain Injury Association of America, approximately 5.3 million Americans currently live with a permanent brain injury-related disability.
Recovery rates following a brain injury can vary significantly based on various factors, including the type and severity of the injury, the individual's overall health, and access to appropriate medical care and rehabilitation services. Here's an overview of recovery rates for common types of brain injuries:
Recovery rates for mild traumatic brain injuries (mTBIs) or concussions are generally favorable, with many individuals experiencing symptom resolution within days to weeks.
According to the Brain Injury Association of America, approximately 85-90% of individuals with mTBIs recover fully within three months post-injury.
However, some individuals may experience persistent symptoms, such as headaches, dizziness, or cognitive difficulties, known as post-concussion syndrome, which can prolong recovery.
Recovery rates for moderate to severe traumatic brain injuries vary significantly depending on the extent of the brain damage and the presence of associated complications. According to the CDC, the five-year approximate outcomes of patients with TBI are as follows:
These recovery rates provide a general understanding of the outcomes associated with different types of brain injuries, but it's important to recognize that individual recovery trajectories can vary widely based on unique circumstances and factors.
Recovery rates following a stroke, which is a type of non-traumatic brain injury, can vary depending on factors such as the location and extent of the brain damage, the type of stroke (ischemic or hemorrhagic), and the timeliness of medical intervention.
Northwestern Medicine reports that about 10% of stroke survivors recover almost completely, while an additional 25% experience minor impairments with little to no disability.
However, approximately 40% of stroke survivors require special care, and 10% require long-term care in a nursing home or other facility.
Several factors can influence the recovery process following a brain injury. Age is one such factor, with younger individuals often demonstrating better recovery outcomes compared to older adults.
Additionally, the timing and intensity of rehabilitation interventions can play a significant role in facilitating recovery and minimizing long-term disabilities. Other factors, such as the presence of pre-existing medical conditions, access to social support networks, and socioeconomic status, can also impact an individual's recovery trajectory.
Understanding these factors can help healthcare professionals, caregivers, and individuals with brain injuries optimize the recovery process and improve outcomes.
A comprehensive approach that addresses physical, cognitive, emotional, and social aspects of recovery is essential for promoting rehabilitation and maximizing quality of life following a brain injury.
Looking for the best neuro rehab near me? Look no further! At NeuLife Rehab, we pride ourselves on being the top choice for individuals recovering from brain injuries and other catastrophic conditions.

With our unwavering commitment to excellence, state-of-the-art facilities, and round-the-clock care, we provide unparalleled support to patients on their journey to recovery.
Our team of highly skilled and compassionate professionals specializes in providing the following programs:
Contact us today at 352-675-2059 to learn more about our programs and how we can help you or your loved one on the path to recovery.
Experience the Neulife difference and discover a brighter, more hopeful future with us.
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare providers with any questions or concerns you may have regarding your health.
Catastrophic injuries can devastate the individual and their loved ones. In the United States, there are 24 million physician office visits for unintentional injuries, and 200,000+ of those lead to death. These types of injuries can occur in various ways, and their effects can manifest differently.
This blog will explore the different types and causes of catastrophic injuries and their long-term effects. By understanding the gravity of these injuries, we can better prepare ourselves and our loved ones for potential accidents and take necessary precautions. Let's dive in and gain a better understanding of catastrophic injuries.
Catastrophic injuries are severe injuries that typically result in permanent disabilities or long-term impairments. Unlike minor injuries such as sprains or bruises, catastrophic injuries often have devastating consequences that can affect a person's ability to perform daily tasks, work, and enjoy life as they did before the injury.
Understanding the types of catastrophic injuries is crucial for prevention, preparedness, and seeking appropriate medical care. This guide will simply discuss the various types of catastrophic injuries.
TBI occurs when a severe blow or shock is delivered to the head, disrupting normal brain function. Symptoms may vary from mild concussions to severe cognitive impairments, affecting memory, speech, and motor skills. TBIs can result from accidents, falls, or sports injuries.
SCI occurs when the spinal cord is damaged, disrupting communication between the brain and the body. These injuries often lead to paralysis or loss of sensation below the injury site. Common causes include car accidents, falls, or acts of violence.
Amputations involve the partial or complete removal of a limb due to severe trauma or medical necessity. Catastrophic accidents such as industrial mishaps, severe car crashes, or explosions can result in traumatic amputations, profoundly impacting mobility and quality of life.
Severe burns result from exposure to flames, chemicals, electricity, or hot surfaces, causing extensive damage to skin and tissues. Burns can lead to pain, infections, scarring, and in severe cases, organ damage or death. Accidental fires, workplace accidents, or explosions are common causes.
It occurs when there are two or more broken bones in the body, often as a result of high-impact accidents like car crashes or falls from heights. These injuries can be complex, requiring extensive medical intervention such as surgery, rehabilitation, and long-term care.
Catastrophic accidents can cause severe damage to internal organs such as the heart, lungs, liver, or kidneys. Blunt force trauma or penetrating injuries can lead to internal bleeding, organ failure, or the need for emergency surgery. Prompt medical attention is crucial to prevent complications.
Catastrophic injuries can also result in permanent vision or hearing loss, significantly impacting daily functioning and quality of life. Traumatic incidents such as explosions, head injuries, or exposure to loud noise can cause irreparable damage to sensory organs.

Catastrophic injuries can have life-altering consequences, impacting individuals physically, emotionally, and financially. Understanding the root causes of these injuries is crucial for prevention and raising awareness.
Catastrophic injuries can have devastating consequences that extend far beyond the initial incident. Let’s examine the long-term effects of catastrophic injuries.
Catastrophic injuries often lead to chronic pain and disabilities that can last a lifetime. Whether it's a spinal cord injury, traumatic brain injury, or an amputation, individuals may face ongoing physical limitations that affect their mobility, independence, and quality of life.
Beyond the physical result, catastrophic injuries can have a significant result on one's mental health. Feelings of depression, anxiety, and post-traumatic stress disorder (PTSD) are common among survivors. Coping with the emotional fallout of such injuries can be challenging, requiring support from mental health professionals, friends, and family members.
The financial implications of catastrophic injuries can be overwhelming. Medical expenses, rehabilitation costs, and ongoing care can quickly accumulate, significantly burdening individuals and their families. Additionally, many survivors may face challenges returning to work or securing employment due to their injuries, further exacerbating financial strain.
Catastrophic injuries can strain relationships with family members, friends, and romantic partners. The caregiving responsibilities placed on loved ones can create tension and stress, while changes in roles and responsibilities may alter dynamics within relationships. Both survivors and their support networks need to communicate openly and seek professional assistance if required.
Survivors of catastrophic injuries may be at increased risk of developing long-term health complications. For example, individuals with spinal cord injuries may face secondary health issues such as pressure ulcers, urinary tract infections, and respiratory problems. Managing these complications requires ongoing medical care and vigilance.
Catastrophic injuries can have far-reaching consequences that impact every aspect of an individual's life. From physical challenges to emotional struggles and financial strain, the long-term effects of these injuries are profound. However, with the proper support, resources, and resilience, individuals can adapt and thrive despite their challenges.
Discover practical techniques for managing catastrophic injuries, from initial assessment to long-term care. Empower yourself with effective strategies.
Effective treatment strategies for catastrophic injuries are crucial for recovery. Victims can regain independence and improve their quality of life by prioritizing prompt medical intervention, personalized rehabilitation plans, and ongoing support. Early intervention is critical to maximizing outcomes and restoring hope for those facing life-altering injuries.
Are you or a loved one facing the challenges of catastrophic injuries? At NeuLife Residential Post-Acute Programs, our expert team is dedicated to helping individuals like you navigate these challenges, empowering you to regain independence and embrace a fulfilling future.
From spinal cord injuries to traumatic brain injuries, we offer comprehensive rehabilitation services such as rehabilitation for brain injury. Plus, learn about our post-acute rehabilitation program aimed at returning patients who have suffered severe injuries back as close as possible to their pre-injury state.
Consult now! Let NeuLife be your partner in recovery.
***
The material on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions or concerns you may have regarding your health.
Traumatic brain injury can have profound and lasting effects on an individual's life. Whether it's from a car accident, a fall, or a sports-related injury, navigating the road to recovery after a brain injury requires patience, diligence, and the right knowledge.
In this comprehensive guide, we'll explore essential tips to aid in TBI recovery and highlight common pitfalls to avoid along the way.
Recovery from a traumatic brain injury requires a comprehensive approach that addresses physical, cognitive, emotional, and nutritional needs.

Patients can maximize their chances of achieving meaningful improvements in function and quality of life by practicing these essential tips:
Physical rehabilitation plays a crucial role in TBI recovery, helping individuals regain mobility, strength, and independence.
Active participation in physical therapy exercises promotes neuroplasticity, the brain's ability to reorganize and form new connections. These exercises may include:
Cognitive rehabilitation focuses on improving cognitive skills such as memory, attention, problem-solving, and executive function.
Through targeted exercises and strategies, individuals can enhance cognitive abilities and overcome challenges posed by TBI. Cognitive rehabilitation techniques may include:
Engaging in cognitive rehabilitation activities regularly can lead to noticeable improvements in cognitive function and overall quality of life.
Proper nutrition and hydration are essential for supporting the body's healing processes and optimizing TBI recovery.
A well-balanced diet rich in vitamins, minerals, antioxidants, and omega-3 fatty acids can provide the nutrients needed for brain repair and regeneration. Key dietary recommendations for TBI recovery include:
Allowing time for rest and avoiding overexertion is essential for preventing fatigue and minimizing the risk of exacerbating symptoms.
Pacing activities involves breaking tasks into manageable segments and taking breaks as needed, helping to conserve energy and avoid overwhelming the brain's capacity to process information.
Many individuals experience feelings of depression, anxiety, frustration, and isolation during the recovery process. Seeking emotional support and mental health care is essential for addressing these challenges and promoting overall well-being. Strategies for emotional support and mental health care include:
Stress management techniques such as deep breathing, relaxation exercises, and mindfulness meditation help reduce stress levels and promote emotional well-being.
By learning to manage stress effectively, you can improve resilience, cope with challenges more effectively, and maintain a positive outlook on your recovery journey.
Following medical advice ensures that you receive appropriate care and support tailored to your specific needs, helping to optimize recovery outcomes.
This involves adhering to the treatment plan prescribed by your doctor which may include medications, therapies (such as physical, occupational, and speech therapy), and attending scheduled follow-up appointments.
Maintaining a positive outlook and being patient with yourself as you progress through recovery is essential for maintaining motivation and resilience.
Celebrating small victories and milestones along the way can boost confidence and reinforce progress, even when challenges arise.
After a brain injury, there are several things to avoid to promote recovery and minimize the risk of complications.
Some examples include:
Patients can optimize outcomes and promote a smoother and more successful recovery journey by avoiding these pitfalls and adopting a cautious and proactive approach to recovery.
Looking for the best neuro rehab near me? Look no further! At NeuLife Rehab, we're dedicated to empowering individuals with traumatic brain injury and other neurological disorders to reclaim their lives and achieve their fullest potential.

As a premier rehabilitation facility, we offer unparalleled programs and services tailored to meet the unique needs of each patient, setting the standard for excellence in neurological rehabilitation. Some of the programs we offer include:
Learn more about how NeuLife Rehab can help you or your loved one on the journey to recovery. Contact us today at 352-660-1411.
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare providers with any questions or concerns you may have regarding your health.
Brain injuries can significantly impact a person's life, often resulting in physical, cognitive, and emotional challenges. However, one aspect often overlooked is the effect on social communication skills. After a brain injury, individuals may struggle to express themselves, understand social cues, and form meaningful connections. These challenges can lead to feelings of isolation, frustration, and even depression.
In this blog, we will explore the impact of brain injuries on social communication skills and provide valuable insights and tips for individuals, their loved ones, and caregivers to navigate this aspect of recovery effectively. Whether you or someone you know has experienced a brain injury or simply want to understand the topic better, keep reading to discover more.
Let’s explore the different ways a brain injury can affect a person:
One of the most noticeable and immediate effects of a brain injury is physical impairment. This can manifest in various ways, depending on the severity and location of the injury. In severe brain injuries, a person may experience paralysis or weakness in their limbs, difficulty with coordination or balance, and changes in sensory perception. These physical effects can significantly impact a person's daily activities and ability to work and perform self-care tasks.
The brain is responsible for processing and interpreting information, so any injury to this crucial organ can result in cognitive difficulties. This can include problems with memory, attention, and executive functioning skills such as planning, problem-solving, and decision-making. A person with a brain injury may struggle with learning new information, managing time, and completing complex tasks. These cognitive effects can significantly impact a person's ability to work, communicate, and maintain relationships.
A brain injury can also significantly impact a person's emotional well-being. Many individuals with brain injuries experience changes in their mood, including depression, anxiety, and irritability. This can be due to the physical and cognitive challenges they face, as well as the emotional adjustment to their injury. Furthermore, a brain injury can also cause changes in a person's personality and behavior, leading to strained relationships and social isolation.

The short answer is yes. Let's delve into why and how.
When someone experiences a brain injury, it can have a significant impact on their social skills. Depending on the severity and location of the injury, individuals may have difficulty understanding social cues, making appropriate social judgments, and expressing themselves effectively. This can lead to challenges in forming and maintaining relationships, participating in conversations, and interpreting nonverbal communication.
A brain injury can also alter one's personality and emotional regulation, affecting social interactions. Seeking rehabilitation and utilizing strategies to improve communication and socialization can significantly enhance an individual's quality of life post-brain injury.
Individuals who have experienced a brain injury often face a myriad of challenges in their daily lives. These individuals may struggle to adapt and cope with their new reality. Let’s explore some common challenges individuals face with brain injury:
For those who have suffered a brain injury, developing and improving social communication skills can be crucial in navigating daily interactions and relationships. Here are five strategies that can help improve social communication skills after a brain injury.
Living with a brain injury can be isolating, and it can feel like no one understands what you are going through. Joining support groups for individuals with brain injuries can provide a sense of community and understanding. It can also be an excellent opportunity to practice social communication skills in a safe and supportive environment.
Advancements in technology have made it easier for individuals with brain injuries to communicate and socialize. For example, speech-to-text software can help those with speech impairments communicate more effectively. Social media platforms also provide a way to connect with others and practice social communication skills at one's own pace.
Speech therapy can be incredibly beneficial for individuals with brain injuries. A speech-language pathologist can work with you to improve communication skills such as verbal expression, understanding of others, and nonverbal communication. These skills not only aid in social interactions but also in daily tasks and activities.
Active listening is a crucial communication skill that involves fully engaging with the speaker and giving them your undivided attention. This skill can be challenging for individuals with brain injuries, but practicing active listening can significantly improve social communication. Start by making eye contact, refraining from interrupting, and summarizing the speaker's words to ensure understanding.
Improving social communication skills after a brain injury is a continuous process, and it is essential to set realistic goals. Break down larger goals into smaller, achievable steps and celebrate progress. This approach can help build confidence and motivation, making it easier to work towards long-term goals.
If you’re searching online for a neuro rehab near me, trust NeuLife Residential Post-Acute Programs for expert care on unlocking social skills after a brain injury and improving your communication. Our team of dedicated professionals understands the complex nature of brain injuries and specializes in creating personalized treatment plans that target social communication impairments.
Whether it's difficulty with nonverbal cues, social situations, or understanding social norms, our therapists use evidence-based techniques to address these challenges and help you rebuild your ability to connect with others.
NeuLife offers a comprehensive range of programs, including:
Don't let a brain injury keep you from socializing and connecting with others—Trust NeuLife to help you navigate the journey to improved social communication skills. Contact us today for a consultation and take the first step towards a brighter, more connected future.

***
The material on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions or concerns you may have regarding your health.
Traumatic brain injury emerges as a distinct and often life-altering experience. It casts a long shadow over one's health, and the journey doesn’t end after hospitalization and discharge. Rather, it introduces a new chapter—one that holds profound implications for cognitive health.
Read on below as we unravel the complexities of TBI and discuss the significance of the hospitalization phase and its link to the risk of dementia.
Traumatic brain injury (TBI) refers to a disruption in normal brain function resulting from an external force. This force can be caused by various incidents, such as accidents, falls, or sports injuries.
From mild concussions to severe brain trauma, the spectrum of TBI is vast, encompassing a range of physical and cognitive consequences, such as:
The severity of traumatic brain injury is a significant factor that can impact the risk of dementia. Research studies have consistently shown that individuals who experience a moderate to severe TBI are at a higher risk of developing dementia later in life compared to those with mild or no TBI.
The gravity of TBI extends beyond the initial incident, with hospitalization playing a pivotal role in the trajectory of recovery. During this phase, medical professionals address immediate concerns, from stabilizing patients to monitoring vital signs.
However, it is not just about the physical recuperation; TBI hospitalization sets the stage for potential cognitive issues that may emerge in the weeks, months, or even years following the injury.
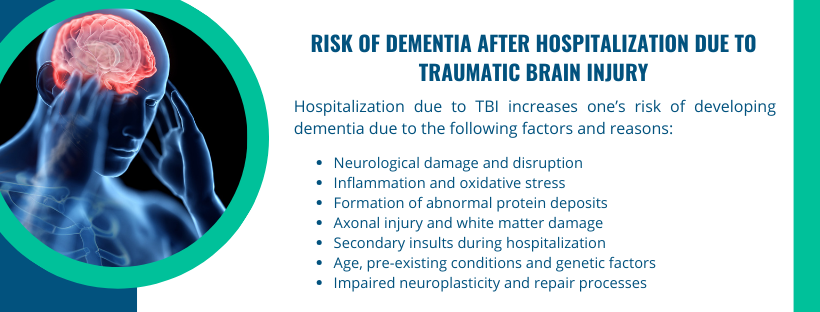
The increased risk of dementia after hospitalization due to TBI is a complex phenomenon with multiple contributing factors. While the exact mechanisms are not fully understood, several vital factors may help explain the heightened risk:
The primary factor contributing to the increased risk is the extent of neurological damage and disruption caused by the traumatic brain injury itself. Severe TBIs can result in significant damage to brain tissue and neural connections.
Traumatic brain injury triggers an inflammatory response in the brain, leading to increased production of pro-inflammatory cytokines.
Chronic inflammation, along with oxidative stress, contributes to ongoing damage and may set the stage for neurodegenerative processes associated with dementia.
TBI has been linked to the accumulation of abnormal proteins in the brain, such as tau and beta-amyloid. These protein deposits are also characteristic of neurodegenerative disorders like Alzheimer's disease, a common cause of dementia.
TBI often involves axonal injury, affecting the long projections of nerve cells responsible for communication between different parts of the brain. White matter damage from TBI can disrupt neural connectivity and contribute to cognitive impairment.
While hospitalization is crucial for the initial management of TBI, certain aspects of the hospital environment may contribute to additional stress on the brain.
Secondary insults, such as complications during surgery, infections, or issues related to intensive care, can exacerbate the overall impact on brain function.
Age at the time of injury is a significant modifier of dementia risk. Older individuals are generally more vulnerable to the long-term effects of TBI. Hospitalized older adults may experience challenges in recovery and may be more susceptible to cognitive decline.
Individuals with pre-existing health conditions or a genetic predisposition to neurodegenerative diseases may face an elevated risk of dementia following TBI. The interaction between TBI and existing vulnerabilities can amplify the overall risk.
TBI can impair neuroplasticity, the brain's ability to reorganize and adapt. This may hinder the brain's natural repair processes, making it more challenging for the neural network to recover and protect against cognitive decline.
While the risk of dementia after traumatic brain injury is a concern, some strategies and interventions can be implemented to potentially mitigate this risk and support cognitive health. Here are several approaches to consider:
Prompt initiation of rehabilitation and treatment following TBI can be crucial. Physical, occupational, and speech therapy, tailored to the individual's needs, can aid recovery and minimize long-term cognitive consequences.
Cognitive rehabilitation focuses on improving specific cognitive functions affected by TBI, such as memory, attention, and problem-solving. These programs aim to enhance neural plasticity and functional recovery.
Additionally, keeping the brain engaged through mentally stimulating activities can support cognitive function. Activities such as puzzles, games, and learning new skills contribute to maintaining cognitive reserves.
Regular physical exercise has been associated with cognitive benefits. It promotes overall brain health, improves blood flow, and supports neuroplasticity. Individuals recovering from TBI should engage in appropriate and supervised exercise programs.
Adopting a healthy lifestyle is crucial. This includes maintaining a balanced diet, staying hydrated, getting sufficient sleep, and avoiding substance abuse. These factors contribute to overall well-being and may positively impact cognitive health.
Regular check-ups and follow-up care with physicians are vital. Ongoing monitoring allows for the identification of any emerging issues and ensures timely intervention.
While the above-mentioned strategies can contribute to mitigating the risk of dementia, it's important to consult specialists for personalized advice and guidance based on individual circumstances.
Are you or a loved one on the path to recovery after a traumatic brain injury?
At NeuLife, we understand that the journey to healing is unique, and we're here to offer comprehensive post-acute rehabilitation to empower individuals facing TBI, spine injuries, amputations, serious orthopedic injuries, strokes, and neurological disorders.

Consult with our experienced physicians and physical therapists at NeuLife to explore personalized strategies aimed at mitigating the risk of dementia post-TBI.
Our team is dedicated to staying at the forefront of rehabilitation science, ensuring you receive the latest and most effective interventions.
Take the first step towards a brighter future. Contact us now at 352-675-2059 or visit our neuro rehab facility!
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare providers with any questions or concerns you may have regarding your health.
Brain injuries are more common than we realize. Car accidents and sports injuries can happen to anyone at any time. And while we often focus on the immediate impact of these injuries, the long-term consequences cannot be ignored. These unforeseen consequences can significantly affect a person's quality of life and ability to function daily.
In this blog post, we will dive into the often-overlooked long-term effects of brain injuries and how they can shape a person's future. Whether you or a loved one has suffered a brain injury or you simply want to understand the potential long-term repercussions, this article is a must-read.
So, let's explore the lasting impact of brain injuries and why raising awareness about their long-term effects is crucial.
Brain injuries are one of the most common and devastating types of injuries. They can have a lasting impact on a person's physical, cognitive, and emotional well-being. According to a study, over 1.7 million Americans sustain a traumatic brain injury each year, with adolescents between ages 15 and 19 and adults age 65 and older among the most likely to sustain a traumatic brain injury.
Brain injury is a broad term for any brain damage caused by external or internal factors. It can be classified into two types:
Brain injury can be caused by a variety of factors, including accidents, violence, and medical conditions. According to the Centers for Disease Control and Prevention (CDC), falls are the leading cause of TBI, accounting for approximately 50% of all cases.
Brain injuries can have long-lasting effects that may not become apparent until years later. These effects can range from cognitive difficulties to changes in behavior and mood. The damage caused by a brain injury can impact a person's daily life, relationships, and overall well-being.
It is crucial to seek medical attention and follow the recommended treatment plan after a brain injury to prevent or minimize long-term problems. If you or a loved one has experienced a brain injury, it is essential to continue monitoring for any emerging issues to ensure proper care and management.

Let us explore the long-term effects of brain injuries, their impact on daily life, and how to manage and cope with them.
One of the most apparent long-term effects of brain injuries is physical impairment. Depending on the severity and location of the injury, it can affect a person's motor skills, balance, coordination, and senses. The physical effects can range from mild to severe and may include difficulty walking, chronic pain, seizures, paralysis, and loss of sensation.
Brain injuries can also result in cognitive impairments that affect a person's ability to think, reason, and process information. These can range from mild difficulties with attention and concentration to more severe impairments in memory, language, and problem-solving. These cognitive impairments can significantly impact a person's daily life, making tasks such as work, school, and even self-care challenging.
Brain injuries can also cause emotional and behavioral changes, which can be distressing for both the person with the injury and their loved ones. These changes can include mood swings, irritability, anger outbursts, impulsivity, and difficulty regulating emotions. These changes can affect relationships, work, and other aspects of daily life.
The long-term effects of brain injuries can significantly impact a person's daily life. It can make it challenging to perform simple tasks, such as getting dressed, cooking a meal, or driving. It can also affect a person's ability to maintain relationships, work, and engage in hobbies and activities they once enjoyed.
Coping with these long-term effects of a brain injury can be a challenging and overwhelming journey, but with the proper support and strategies, navigating these changes and living a fulfilling life is possible.
So, let's dive in and start finding ways to cope with the long-term effects of brain injuries together.
The first step in coping with the long-term effects of a brain injury is to seek professional support. A team of healthcare professionals, including doctors, therapists, and counselors, can provide emotional and physical support and help you manage your symptoms. They can also guide you and your loved ones on strategies to cope with the long-term effects.
Physical activity plays a crucial role in coping with the long-term effects of brain injuries. Exercise helps improve strength, mobility, and balance, which can be affected by a brain injury. It also releases endorphins, which can improve mood and alleviate symptoms of depression and anxiety.
Cognitive rehabilitation is a therapy that focuses on improving cognitive skills, such as memory, attention, and problem-solving, after a brain injury. Working with a cognitive therapist can help you develop techniques and strategies to manage these changes. Cognitive rehabilitation may also involve using technology or other tools to help compensate for any cognitive difficulties.
Living with the long-term effects of a brain injury can be overwhelming, and it is essential to find healthy coping mechanisms to manage the stress. This can include relaxation techniques, such as deep breathing or meditation, joining a support group, talking to a trusted friend or family member, or finding a creative outlet like painting or writing.
Taking care of your overall health is crucial when coping with the long-term effects of a brain injury. This includes getting enough sleep, eating a nutritious diet, and avoiding alcohol and drugs. A brain injury can increase the risk of developing other health conditions, such as high blood pressure and diabetes, so it is essential to attend regular check-ups and follow your doctor's recommendations.
Educating yourself and others about the long-term effects of brain injuries is essential. This can help you understand your condition better and advocate for yourself. It can also help those around you, such as family, friends, and co-workers, understand your needs and provide you with the necessary support.
Are you or a loved one struggling with the long-term effects of a brain injury? Don't let the unforeseen consequences of this life-altering event control your future. The first step towards recovery and a better quality of life is enrolling in NeuLife’s post-acute rehabilitation program.
Our specialized program offers a comprehensive and personalized approach to traumatic brain injury rehabilitation, focusing on physical, cognitive, emotional, and behavioral therapies. Our program addresses the unique challenges and complications of brain injury.
At NeuLife, we understand that the journey to recovery is long and challenging, so we provide a supportive and nurturing environment for our patients. So, if you’re looking online for a trusted “neuro rehab near me,” look no further than the NeuLife Residential Post-Acute Program.
Contact us today to learn more and take the first step toward reclaiming your life.
***
The material on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions or concerns you may have regarding your health.
Left-side brain damage can be a life-altering event, impacting various aspects of cognition and function. This blog will delve into the recovery process, offering insights and guidance for those on this challenging journey.
The brain's left hemisphere plays a crucial role in controlling the right side of the body and is primarily responsible for language processing and analytical thinking.
When damage occurs in this region, it can lead to a variety of cognitive and motor impairments. The consequence can be diverse and may include one or more of the following:
It's important to note that the effects of left-side brain damage can vary widely from person to person.
Left hemisphere brain injuries can be caused by a variety of factors, ranging from sudden traumatic events to progressive degenerative conditions. Understanding the different causes is crucial for both prevention and effective management of these injuries. Here are some common causes of left-hemisphere brain injuries:
Understanding the underlying cause of left-hemisphere brain injuries is essential for accurate diagnosis and appropriate treatment. Early intervention, rehabilitation, and medical management are key components of addressing the diverse effects of these injuries.
Left-side brain damage triggers a cascade of events in the immediate aftermath, necessitating prompt medical attention and intervention. Here’s what can happen after the initial impact:
In cases of trauma, a rapid medical response is essential. Emergency medical services will assess the individual's condition, stabilize vital signs, and transport them to the hospital.
Upon admission to the hospital, diagnostic imaging, such as computed tomography (CT) or magnetic resonance imaging (MRI), is performed to identify the location and extent of the left hemisphere brain damage.
Neurologists conduct a thorough examination to assess motor skills, sensory function, and cognitive abilities. This initial assessment helps identify the specific deficits resulting from left-side brain damage.
Treatment strategies aim to minimize secondary damage and support brain function. Depending on the cause (e.g., stroke, trauma), interventions may include clot-dissolving medications, surgery to address bleeding, or other targeted therapies.
Embarking on the recovery process after left-side brain damage is a multifaceted journey that demands patience, resilience, and a comprehensive approach.
The path to recovery is unique for each individual, influenced by factors such as the type and severity of the injury, the effectiveness of medical interventions, and the individual's overall health. Here's what to expect during the recovery process:
Once medically stable, individuals are introduced to rehabilitation programs, often involving physical, occupational, and speech therapy.
Therapists will collaborate with the patient to set realistic short-term and long-term goals based on their unique challenges and potential for recovery.
Physical rehabilitation will focus on improving motor skills, coordination, and balance. There will also be an introduction of adaptive tools and techniques to accommodate motor challenges.
Rehabilitation efforts address cognitive deficits, including memory impairment, through targeted exercises. Therapists may use external memory aids, such as calendars and reminders, to support memory function.
Speech therapy targets language deficits, including expressive and receptive aphasia. There’s also an integration of communication strategies to improve language skills and social interaction.
Recovery is seldom a linear process. Challenges and setbacks are an inevitable part of the journey. Cognitive fatigue, frustration, and the plateau effect can dampen spirits. Acknowledging these obstacles and developing resilience strategies are critical components of the recovery process.
Therapists will integrate interventions to address the emotional challenges associated with the recovery process. They will also collaborate with mental health professionals when necessary to provide additional emotional support.
Recovery is not a solitary endeavor; it requires a robust support system. Family and friends play a pivotal role in the healing process. Their encouragement, understanding, and active involvement in therapies contribute significantly to the individual's motivation and progress.
Regular assessments are conducted to evaluate progress and adjust rehabilitation goals. Ongoing communication with the interdisciplinary team ensures a collaborative and adaptive approach.
Patients will be gradually reintroduced to community settings and home-based exercises that mimic daily life situations. Doctors will provide recommendations for home modifications to facilitate independence and safety.
The ultimate goal of the recovery process is to reintegrate into daily life. This involves not just physical recovery but also psychological adjustment.
Learning to navigate the 'new normal' often involves vocational rehabilitation, counseling, and ongoing medical support. It's a holistic approach that aims at restoring not just abilities but a sense of purpose and self.
The patient’s medical team will implement long-term strategies to maintain progress and independence. There will also be periodic reassessments to monitor ongoing progress and adjust therapy goals as needed.
Lastly, there should be continuous communication with the healthcare team to address any emerging challenges or opportunities for improvement.

At NeuLife, we redefine the standards of rehabilitation for brain injury, offering a sanctuary of healing for individuals facing the challenges of traumatic brain injuries (TBI), spine injuries, serious orthopedic injuries, strokes, and neurological disorders.
Our commitment to providing exceptional care extends beyond the ordinary – we are dedicated to empowering lives, restoring independence, and fostering hope.
Contact us now at 352-492-3475 or visit our post acute rehabilitation center to know more.
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare providers with any questions or concerns you may have regarding your health.
Physical activity is something that most of us take for granted. We use our bodies and move around without even thinking twice about it. But for people with a Spinal Cord Injury (SCI), physical activity can seem like an impossible task. However, it is crucial for their overall health and well-being.
In this blog, we will delve into the world of physical activity for people with spinal cord injury and how it can improve their quality of life. So whether you have a spinal cord injury or know someone who does, keep reading to learn about the benefits of staying active and how it can change lives.
Let’s explore the numerous physical and psychological benefits of regular physical activity for people with SCI and why it should be an integral part of their daily routine.
Individuals with SCI often have impaired cardiovascular function due to decreased muscle mass and reduced physical activity. Regular physical activity can help improve and maintain cardiovascular health, reducing the risk of heart disease and stroke. Additionally, it can also help prevent blood clots, which are a common complication for people with SCI.
Spinal cord injury can lead to muscle strength and mass loss, reducing endurance and increased fatigue. Regular exercise, precisely strength and resistance training, can help increase muscle mass and improve overall muscle strength. This allows individuals with SCI to regain their physical abilities and makes daily activities such as transfers and wheelchair propulsion easier.
People with SCI often struggle with weight management due to a reduction in energy expenditure and the tendency to lead a more sedentary lifestyle. Being overweight or obese can increase the risk of health complications such as heart disease and diabetes. Physical activity can help individuals with SCI maintain a healthy weight and reduce their risk of these conditions.
Bone density can decrease rapidly in individuals with SCI due to the lack of weight-bearing activities. This can increase the risk of bone fractures and other bone-related problems. Physical activity, particularly weight-bearing exercises, can help improve bone density and reduce the risk of osteoporosis.
Living with a spinal cord injury can have a significant impact on an individual's mental health. Depression, anxiety, and social isolation are common among people with SCI. Regular physical activity can help alleviate the symptoms of these conditions and improve overall mood and self-esteem. It can also provide a sense of accomplishment and empowerment, benefiting individuals with SCI.
Physical activity releases endorphins, also known as the "feel-good" hormones, which can help reduce stress and improve overall well-being. This is especially important for people with SCI, who may experience higher levels of stress related to their injury and the challenges it brings. Engaging in regular physical activity can help promote relaxation and reduce stress levels.
People with SCI are at a higher risk of secondary health complications, such as respiratory infections, bladder and bowel dysfunction, and pressure ulcers. Regular exercise can help prevent or manage these complications, improving overall health and quality of life.
If you or a loved one have an SCI, do not hesitate to consult with a healthcare professional to create a personalized exercise plan and start reaping the physical and mental benefits of staying active.

There are various types of physical activity that people with SCI can engage in depending on their injury level, severity, and overall health condition, and here are some of those:
Some examples of low-impact cardiovascular exercises that people with SCI can engage in include using a stationary hand bike, wheelchair rolling, or swimming. These activities can be modified to suit the individual's level of injury and fitness level, making them accessible to everyone.
One of the most common types of strength training for people with SCI is weightlifting using resistance bands or machines that target specific muscle groups. Working with a physical therapist to design a strength training program suitable for the individual's injury level and muscle strength is essential.
Some examples of flexibility exercises include stretching, yoga, or pilates. These exercises can be done with or without the assistance of a physical therapist, depending on the individual's level of injury.
Balance and coordination exercises for people with SCI include functional activities like sitting to standing, standing in place, or using balance boards or stability balls. Again, these exercises can be modified based on the individual's level of injury.
For people with SCI, incorporating mind-body exercises into their routine can also improve body awareness, reduce spasticity, and promote relaxation.
Take back control of your life with the power of physical activity for spinal cord injury at NeuLife – the leading clinic that offers spinal cord injuries rehabilitation and rehabilitation for brain injury.
Due to SCI's unique challenges and limitations, it is essential to approach physical activity with caution and careful planning. Here are the top 5 considerations for safe physical activity with spinal cord injury.
Take control of your recovery journey and enhance your quality of life with NeuLife's post-acute rehabilitation programs for people with spinal cord injury. Through tailored physical activity plans, our expert team will guide and support you in regaining strength, independence, and confidence.
Aside from that, we also offer industry-leading neuro rehabilitation, helping to support those recovering from brain injuries and spinal cord injuries. Our tailored approach is designed to address each individual's unique needs, maximizing their potential for recovery.
Don't let your injury hold you back. Join us at NeuLife and experience the power of physical activity in overcoming obstacles and achieving your goals. Contact us to start your personalized program and embrace a fulfilling life after a spinal cord injury.

***
The material on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions or concerns you may have regarding your health.
Global anoxic brain injury is a complex medical condition that results from a severe lack of oxygen to the brain. This oxygen deprivation can lead to neurological issues and cognitive impairments, affecting an individual's overall quality of life.
In this comprehensive blog post, we will delve into the causes, symptoms, management, and rehabilitation strategies for GABI.

Understanding this condition is crucial for patients, their families, and healthcare professionals, as it can pave the way for early diagnosis, effective treatment, and the best possible outcomes.
Global anoxic brain injury, or GABI, is a specific type of brain injury characterized by a widespread lack of oxygen to the brain. This can occur due to various reasons, including cardiac arrest, choking, or drowning.
When the brain is deprived of oxygen, it can lead to a cascade of events that damage brain cells and affect brain function. Understanding the nature of GABI is essential in addressing its causes, symptoms, and management.
Global anoxic brain injury is also medically known as cerebral anoxia or global ischemia.
Global anoxic brain injury occurs when the brain is deprived of oxygen for an extended period. It is typically caused by the following conditions or instances:
Cardiac arrest is one of the most common causes of GABI. During a cardiac arrest, the heart stops beating, leading to a sudden interruption in the blood flow to the brain. This can result from various heart conditions or other factors.
When the air supply to the brain is cut off due to choking or suffocation, it can quickly lead to oxygen deprivation, causing GABI. This can happen in both adults and children.
Drowning is a critical cause of GABI, especially in cases where a person is submerged in water for an extended period. The lack of oxygen can lead to severe brain injury.
In some cases, drug overdoses, particularly those involving opioids, can result in respiratory failure and GABI. The overdose impairs the body's ability to breathe, leading to oxygen deprivation in the brain.
Severe and prolonged asthma attacks can lead to inadequate oxygen intake and potential oxygen deprivation to the brain.
Extremely low blood pressure, often due to various medical conditions or severe bleeding, can result in reduced oxygen delivery to the brain and contribute to GABI.
The symptoms of GABI can vary widely depending on the severity of the injury and the specific areas of the brain affected. Common symptoms include:

The treatment of global anoxic brain injury is a complex and multifaceted process that involves various medical interventions, therapies, and rehabilitation strategies. Here are some of the key treatment options for GABI:
When a person experiences oxygen deprivation due to anoxia (lack of oxygen), it's crucial to initiate immediate medical interventions to restore oxygen supply to the brain. These interventions may include:
After the initial medical stabilization, healthcare professionals may prescribe medications to manage symptoms, prevent complications, and support brain function. These medications may include:
In some cases, surgical intervention may be necessary to address specific issues associated with GABI. This may include:
Rehabilitation is a critical component of GABI treatment, focusing on helping individuals regain lost functions and improve their quality of life. Different forms of rehabilitation include:
Depending on the extent of the brain injury, individuals may benefit from assistive devices such as mobility aids, communication devices, and adaptive tools to enhance their independence and quality of life.
Emotional and psychological support is essential for individuals with GABI and their families. Support groups, counseling, and other mental health resources can help individuals cope with the challenges of recovery.
In cases of severe GABI, long-term care planning is necessary to address the ongoing needs of individuals with significant cognitive and physical impairments. This may involve home healthcare, skilled nursing facilities, or other specialized care options.
Healthcare professionals will continuously monitor and assess the individual's progress and adjust the treatment plan accordingly. Periodic evaluations can help optimize the care and support provided.
Are you or a loved one in search of the best rehabilitation facility for brain injury and other neurological disorders? Look no further; NeuLife Rehabilitation is your beacon of hope and healing.

At NeuLife, we offer a wide range of services, such as neuro rehab, post acute rehabilitation, stroke rehab, and more. With decades of experience, our board-certified doctors and therapists are dedicated to providing the highest level of care for individuals with brain injuries and neurological disorders.
Your journey to recovery begins at NeuLife. Contact us today at 352-660-1411 and discover the possibilities that lie ahead!
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare providers with any questions or concerns you may have regarding your health.
Head injuries can be scary and overwhelming, especially if accompanied by vomiting. Not only does it add a layer of worry, but it can also be a sign of a more serious issue. This blog will discuss everything you need to know about vomiting after a head injury - what it means, what could be causing it, and, most importantly, how to treat it.
So, if you or someone you know has experienced vomiting after a head injury, keep reading to equip yourself with the knowledge and understanding to handle it effectively.
A head injury refers to any trauma to the head that can cause damage to the brain. It can range from mild injuries like bumps and bruises to severe and life-threatening ones. Injuries to the head can occur due to various reasons, such as falls, accidents, or sports-related activities. Head injuries and physical harm can also result in cognitive and behavioral complications, including nausea and vomiting.
The brain controls all bodily functions, including digestion and physical movement. Therefore, any damage to the brain can lead to a disruption in these functions. After a head injury, the body may struggle to regulate the digestive system, leading to symptoms like vomiting, nausea, and loss of appetite. Additionally, head injuries can also cause changes in the balance and coordination of the body, making it difficult for patients to control their muscle movements, further contributing to vomiting.
Head injuries can occur in various forms - from a simple bump on the head to a severe traumatic brain injury. Along with common symptoms like headache and dizziness, vomiting is common after a head injury. While it may be a natural response to trauma, prolonged and severe vomiting can indicate a more serious condition.
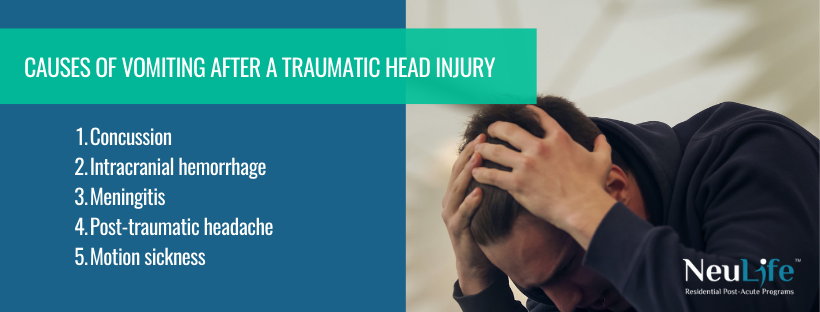
Here are the top five causes of vomiting after a head injury and what you need to know to ensure proper treatment and recovery:
A concussion is one of the most common causes of vomiting after a head injury. Trauma occurs when a person experiences a forceful blow to the head, causing the brain to rush within the skull. This movement can damage brain cells and disrupt the brain's normal functioning, leading to vomiting. The fluid buildup in the brain can also trigger nausea and vomiting.
Intracranial hemorrhage, also known as bleeding inside the skull, is another significant cause of vomiting after a head injury. A blood vessel rupture in the brain can pressure the surrounding tissues, causing symptoms like headache, blurred vision, and vomiting. Intracranial hemorrhage can have severe consequences and even be life-threatening if left untreated.
Sometimes, vomiting after a head injury may be a sign of meningitis. Meningitis is a severe infection that causes inflammation of the protective membranes surrounding the brain and spinal cord. If the head injury has exposed the skull, it can make it easier for bacteria or viruses to enter the brain and cause infection, leading to vomiting, fever, and confusion.
Headaches are a common symptom after a head injury and can also trigger vomiting. When the impact of a head injury causes swelling or inflammation in the tissues surrounding the brain, it can put pressure on the nerves, causing a headache. This type of headache, known as post-traumatic headache, can last for weeks or even months after the injury and can be accompanied by vomiting.
Depending on the location and severity of the head injury, it can also damage the vestibular system - the part of the inner ear that helps with balance and coordination. This damage can lead to symptoms like dizziness, vertigo, and nausea, typical symptoms of motion sickness. If the injury affects the vestibular system, it can trigger vomiting as the body tries to rid itself of the perceived toxins.
Traumatic head injuries, or concussions, are common in today's fast-paced and physically demanding world. While most people may think of them as a temporary inconvenience, the reality is that these injuries can have long-lasting and devastating effects on the brain.
The brain is the control center of our entire body, responsible for our thoughts, emotions, and movements. Any damage to this complex organ can have far-reaching consequences. When it comes to traumatic head injuries, the brain is particularly vulnerable due to its soft and delicate nature.
The impact of traumatic head injuries on the brain cannot be underestimated. Not only does it physically damage brain tissue, but it can also disrupt the brain's communication network, leading to a range of cognitive, emotional, and behavioral changes. These changes can profoundly impact a person's life, affecting their ability to work, socialize, and carry out everyday tasks.
A traumatic head injury can manifest in various ways, from memory loss and poor concentration to mood swings and difficulty processing information. Unfortunately, these effects can last for months or even years, significantly impacting a person's quality of life. It's not just athletes and soldiers at risk of traumatic head injuries; accidents, falls, and physical assaults can also cause them.
This silent epidemic is often overlooked, but it's essential to understand its consequences and take necessary precautions to prevent it. By raising awareness and implementing proper prevention measures, we can minimize the devastating effects of these injuries on individuals, families, and communities. Remember, protecting our brains also means protecting our futures.

Here are some of the most influential and well-researched treatment options for vomiting after a traumatic head injury.
Anti-nausea medication is one of the most common ways to treat vomiting after a traumatic head injury. These medications work by blocking the signals that trigger nausea in the brain. They can come in pills, injections, or suppositories and are typically prescribed by a healthcare professional.
Vomiting can cause dehydration, worsening other symptoms and delaying the healing process. Replacing lost fluids and electrolytes through drinking water and other liquids, such as sports drinks, is essential to combat this. In more severe cases, intravenous (IV) fluids may be necessary to replenish the body's electrolyte levels.
Sometimes, vomiting may result from a lack of oxygen to the brain, causing nausea and other symptoms. In these cases, oxygen therapy can be an effective treatment option. This involves administering oxygen through a mask or nasal cannula to improve oxygen levels and alleviate symptoms.
Changing your diet can significantly manage vomiting after a traumatic head injury. Certain foods and drinks, such as greasy or spicy foods, alcohol, and caffeine, can worsen nausea and vomiting. Sticking to bland, easy-to-digest foods and staying hydrated is essential to minimize the chances of vomiting.
Rehabilitation plays a crucial role in recovering after a traumatic head injury. Depending on the individual's specific needs, this may include physical, occupational, and speech therapy. These post-acute rehabilitation and therapies help regain strength, coordination, and cognitive function, improving overall well-being and potentially reducing vomiting episodes.
In addition to these treatment options, monitoring symptoms closely and seeking medical attention if vomiting persists or other concerning symptoms arise is essential. Recovery from a traumatic head injury is a gradual process and may require a combination of treatments.
Individuals may respond differently to these treatments, so working closely with a healthcare professional to determine the best course of action is essential. With proper care and treatment, individuals can recover from their head injury and resume an everyday, healthy life.
Seeking comprehensive and expert care for post-head injury vomiting? Look no further. NeuLife Rehabilitation, one of Florida’s best brain injury rehabilitation centers, offers specialized treatment and support for those experiencing this often overlooked symptom.
Our dedicated team of specialists at a neuro-rehabilitation center will evaluate your unique needs and tailor a personalized rehabilitation plan to help you overcome vomiting and other lingering effects of a head injury. Want to visit NeuLife Rehabilitation? Schedule a tour today!
Don't let this potentially dangerous and debilitating symptom go untreated – contact NeuLife Rehabilitation today and take the first step towards a brighter, healthier future.
***
The material on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions or concerns you may have regarding your health.
Parkinson's disease is a progressive neurological disorder that affects more than 8.5 million people worldwide. While it's often associated with motor symptoms like tremors and rigidity, its impact extends far beyond the muscles.
In this comprehensive blog post, we will explore how Parkinson's disease affects the brain, delving into the intricate neurological changes that underlie this condition.
Parkinson's disease (PD) is a neurodegenerative disorder that primarily affects movement control. It is a chronic and progressive condition, which means that its symptoms worsen over time.
The disease is characterized by a variety of motor and non-motor symptoms, and it primarily results from the loss of dopamine-producing neurons in a region of the brain called the substantia nigra. Some of its most recognizable motor-related symptoms include:
Parkinson's disease is often thought of as primarily affecting motor function, but it can also have significant cognitive and emotional consequences. This includes memory problems, attention difficulties, mood disorders, sleep disturbances, and more.
The rate of symptom progression varies from person to person. Early-stage symptoms may be mild and easily managed, but motor and non-motor symptoms can become more severe and disabling as the disease advances.
Parkinson's disease primarily affects specific brain structures, leading to the characteristic motor symptoms and other associated changes. The critical brain structures affected by Parkinson's disease include:
The substantia nigra is located in the midbrain and has a high concentration of dopamine-producing neurons. It is mainly responsible for the production of dopamine一a neurotransmitter that acts as a chemical messenger in the brain.
Parkinson’s disease primarily targets the substantia nigra, impairing dopamine-producing neurons and inducing cell death. As dopamine levels decrease, the brain's ability to regulate movement becomes impaired.
The basal ganglia is a complex group of structures deep within the brain, and it plays a crucial role in controlling voluntary motor movements.
In Parkinson's disease, dysfunction in the basal ganglia due to dopamine depletion disrupts the normal balance of excitatory and inhibitory signals, leading to motor impairments. This results in the hallmark symptoms of the disease, such as difficulty initiating and coordinating movements.
In Parkinson's disease, abnormal protein aggregates called Lewy bodies, primarily composed of a protein called alpha-synuclein, accumulate within neurons.
These aggregates disrupt normal cellular function and are believed to contribute to the degeneration of dopamine-producing neurons and other brain cells.
While the cortex is not the primary site of dopamine production, it is influenced by the basal ganglia and plays a role in motor planning and execution. Dysfunction in the cortex contributes to motor difficulties in Parkinson's disease.
This can also result in cognitive changes, including difficulties with memory, attention, and executive functions.
The thalamus is another vital structure affected by Parkinson's disease. It acts as a relay station for sensory information and motor signals between different parts of the brain. Changes in the thalamus can impact motor control and sensory processing.
Parkinson's disease can also affect structures in the limbic system, including the hippocampus, which is involved in memory and emotion. Cognitive and mood-related symptoms in Parkinson's disease are partly attributed to these changes.
The brainstem, which includes the midbrain, pons, and medulla oblongata, contains various nuclei and structures that play a role in autonomic functions, such as blood pressure regulation and digestion.
Dysfunction in these areas can lead to non-motor symptoms like autonomic dysfunction in Parkinson's disease.
The treatment of Parkinson's disease aims to manage its symptoms and improve the quality of life for individuals with the condition. Treatment plans are often tailored to each patient's specific symptoms and needs, and they may include a combination of the following approaches:
Physical therapy can help individuals with Parkinson's improve their mobility, balance, and posture. Occupational therapy focuses on activities of daily living and can assist with fine motor skills, such as handwriting.
Moreover, physical therapy and occupational therapy can play a significant role in promoting neuroplasticity in individuals with Parkinson's disease.
Neuroplasticity is the brain's ability to reorganize and adapt by forming new neural connections throughout life. It is also essential for learning, recovery, and adapting to changes caused by neurological conditions like Parkinson's disease.
Speech therapy can address speech and swallowing difficulties (dysarthria and dysphagia) that may occur in Parkinson's disease.
Regular physical exercise is beneficial for people with Parkinson's. It can improve muscle strength, flexibility, and overall fitness, helping to maintain mobility and delay the progression of symptoms. Activities like walking, swimming, and dancing can be beneficial.
Lifestyle changes can contribute to better overall health and symptom management. Family members and caregivers should help patients practice healthy habits, such as maintaining a balanced diet, staying hydrated, and managing stress,
Non-pharmacological therapies, including music therapy, art therapy, and mindfulness techniques, can help improve mood and overall well-being.
Cognitive rehabilitation for Parkinson's disease is a structured, individualized approach to address cognitive impairments and improve cognitive functioning in individuals with Parkinson’s. Some examples of therapies include:
Are you or a loved one facing the challenges of recovery from traumatic brain injuries (TBI), spinal injuries, and neurological disorders?
NeuLife Rehab is an inpatient facility designed to support your recovery around the clock. Our modern, comfortable accommodation and cutting-edge equipment ensure you receive the highest level of care.

Our experienced medical team is dedicated to providing the support, care, and therapies you need on your journey to recovery.
We offer a wide range of post-acute rehabilitation and neuro rehabilitation services tailored to your unique needs. Whether you require intensive physical therapy, cognitive rehabilitation, or assistance with daily living activities, we have you covered.
Your journey to healing begins here. Contact us now at 352-492-3475.
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare providers with any questions or concerns you may have regarding your health.
It's National Traumatic Brain Injury Awareness Month. Now is the perfect time to look into nutrition therapy to help the brain recover after a traumatic brain injury. Nutrition therapy offers a non-invasive and natural approach to helping the brain overcome this potentially devastating injury.
In this blog, learn how nutrition therapy for TBI can help a brain recover and even benefit those who haven't been diagnosed with TBI. So, let's get started to understand better how nutrition therapy works and how it can help you or someone you love.
Traumatic brain injury or TBI is a severe and sometimes debilitating injury due to a violent blow or jolt to the head. It can result in physical, psychological, cognitive, and/or behavioral deficits. TBI can range from mild to severe and cause loss of consciousness or a prolonged state of being. Common causes of TBI include car accidents, assaults, sports collisions, and falls.
Symptoms may include:
Nutrition is essential to recovery following a traumatic brain injury (TBI). Nutrition therapy helps the brain become healthier and function optimally. It consists of strategies such as eating a balanced diet, consuming specific nutrients, and consuming drugs that help increase nutrient absorption.
A diet with adequate proteins, vitamins, minerals, essential fatty acids, and antioxidants can help the brain get the proper nourishment to recover. Essential vitamins and minerals are needed to provide energy, support neurological functions, and help heal damaged cells. Foods high in protein help the brain repair and create new neurons, while omega-3 fatty acids in fatty fish are essential for optimizing cognitive function.
Following dietary guidelines can ensure the brain receives the proper nourishment to repair existing damage while allowing cells to regrow. With consistent nutrition therapy, the brain can continue to get the essential nutrients it needs for optimal functioning and recovery.
In general, good nutrition is essential for our body and health. But how does it affect our brains? Nutrition plays a massive role in keeping our brain healthy and functioning at its highest capacity.
From infancy to adulthood, good nutrition contributes to proper brain development. A balanced diet with macronutrients and micronutrients aids in brain growth. Macronutrients like proteins, carbohydrates, and fats provide energy and help organs and tissues function. Micronutrients like vitamins and minerals help with metabolic processes and tissue repair. There is a direct correlation between proper nutrition and how it affects cognitive function.
Nutrients, such as omega-3 fatty acids, contribute to cell membranes and improve communication between neurons, positively affecting mental health. Antioxidants in foods like fruits and vegetables protect the brain from damage and prevent dementia and Alzheimer’s. Additionally, a diet low in sugar and processed foods may stimulate areas of the brain associated with attention and executive function.
Adequate hydration is also essential, as it helps the brain function correctly. Dehydration can cause headaches, fatigue, and difficulty concentrating. Our brain needs water to transport chemicals responsible for memory formation and oxygen for energy.
Several different types of nutritional therapy are available for those with traumatic brain injuries.
This type of nutritional therapy typically involves dietary counseling and nutritional guidance tailored to meet the individual’s needs and improve overall brain health.
Sports nutrition therapy helps those with TBI maximize their performance, maintain a healthy body index, and boost their energy levels. It focuses on meal planning, supplementation, hydration, and other health factors.
Mindful eating focuses on helping individuals with TBI become more aware of their hunger signals and emotional responses to food. It also allows the individual with TBI to relax, increase their feelings of control, and build self-confidence around food.
This type of nutritional therapy is designed to identify and address food sensitivities and allergies. It can help those with TBI identify which foods they should avoid and which they should include in their diet to promote physical and mental well-being.
Eating the proper nutrients can help your brain stay healthy and function properly, while a poor diet can put you at greater risk for cognitive decline. Here, we’ll look at how nutrition affects the brain and provide tips for getting the right balance of healthy foods.
Regularly consuming essential vitamins and minerals, such as omega-3 fatty acids, B vitamins, and iron, keeps your brain firing on all cylinders. These essential nutrients assist in the production of neurotransmitters, which promote brain development, cognition, and connection.
With the demands of modern life, having memory and concentration at their peak is key. Regular consumption of omega-3 fatty acids, along with other supplements, can help achieve physical and cognitive performance.
The stress hormone cortisol can damage brain cells over time. Eating a diet rich in vitamin C-containing foods and B vitamins can help reduce cortisol levels and other damaging hormones.
Nutrients like magnesium, omega-3 fatty acids, and B vitamins may reduce the risk of depression and anxiety. Eating foods rich in these vital elements can promote better mental health and reduce your risk of developing mental health issues.
To function correctly, the brain depends on essential nutrients, such as Vitamin A. Vitamin A-containing foods, such as eggs, dairy, and fish, can improve cognitive function and help ensure the brain operates optimally.
Eating a diet loaded with iron, magnesium, B vitamins, and other brain-supporting nutrients can help boost mental stamina and energy, allowing you to better focus on tasks and think more clearly.
By taking care of your nutrition needs, you’ll be able to reap the cognitive benefits of improved brain activity, better memory and concentration, stress reduction, and increased mental stamina. So, consume these essential vitamins and minerals to help keep your brain healthy and functioning correctly.
If you or a loved one have experienced a traumatic brain injury and are trying to recover, Neulife is here to help!
Our team specializes in post-acute rehab to help accelerate the healing process. Thanks to our innovative and comprehensive neuro rehabilitation program, including nutrition therapy, traumatic brain injury rehabilitation, and cognitive therapy, Neulife can help you or a family member unlock the healing potential of the brain and begin the journey to recovery.
Take the first step towards a healthy future. Contact us today and learn how nutrition therapy for TBI can help the brain recover.
***
The material contained on this site is for informational purposes only and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE, and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions or concerns you may have regarding your health.

We know that choosing the next step in your recovery from a catastrophic illness or injury is complex. Together, we can help you take the next step.
Contact us with any questions today.